KUALA LUMPUR, Oct 19 – “I remember one really, really bad experience with a doctor training to be a specialist. He actually shouted at one of my patients in the ward loudly in front of everyone that he deserved to die because of his sins.
“And because of his sins, he got HIV…and therefore he deserves to die…does not deserve any treatment.”
This recollection was made by a medical provider during a survey conducted as part of a study that explored physician’s attitudes and perceptions of transgender and HIV positive patients in Malaysia.
The doctor surveyed continued: “So, it was really bad and traumatising. And the patient actually wrote a letter to the director of the hospital. We had to take action…”
Ryan Sutherland, a researcher from the Yale School of Medicine who conducted the study in collaboration with University Malaysia’s Centre of Excellence for Research in AIDS (CERIA) presented his findings at a webinar organised by the Malaysian AIDS Council last September 15.
He said: “This person (doctor who shouted at the patient) did not pass his specialist exam but he was able to get his qualifications outside of Malaysia (in Singapore) and was able to come back into the country now.”
Sutherland, who has a Masters in Public Health from Yale University, said through the study he interviewed and surveyed primary care and specialist medical providers who provide human immunodeficiency virus (HIV) care to HIV positive and transgender patients in Malaysia and medical trainees (interns/residents, fellows) to better understand barriers and facilitators to prescribing antiretroviral therapy (ART).
The objective of the research was also to assess provider and trainee perspectives on how HIV treatment outcomes and adherence could be improved for transgender patients.
“The rationale for this work is obvious — transgender populations are of particular interest because they have been insufficiently studied and are particularly vulnerable to HIV infection and non-adherence to ART,” he said.
“Globally, transgender populations are disproportionately affected by HIV and Malaysia has one of the highest burdens of HIV in the world so that’s very important for us to investigate.
“Few studies compare the perceptions of both medical and trainee providers, who treat transgender patients, investigating how the training stage might play in the variance of empathy, transphobia, stigma and unwillingness to treat.”
The study surveyed 35 physicians throughout the country from Selangor, Perak, Sabah, Negeri Sembilan, Kelantan, and Kuala Lumpur, and included housemen (four), medical officers (seven), consultants (four), specialists (18), and general practitioners (two).
It involved licensed Malaysian medical doctors trained in Malaysia who have provided HIV care to at least one transgender woman in the last 12 months of the research and currently licensed Malaysian medical trainees trained in Malaysia at the houseman or fellowship level who have provided care to at least one HIV positive transgender woman in the last 12 months of the research.
“Overall this study is important because it will help transgender specific interventions, and to inform those interventions and promote enhanced adherence to ART and highlight opportunities for health systems improvement,” Sutherland said.
“How Do We Find Them? We Don’t Find Them On The Streets…”

Physicians in the study cited a variety of challenges when it comes to treating and prescribing medicine for transgender patients including just a general feeling of discomfort when it comes to treating transgender patients.
This creates a barrier, according to a doctor surveyed, who said that patients would then be referred back to other providers.
Barriers also arise from the perception that trangender people are difficult to locate and connect with.
“There was also this general conception that the transgender community is actually quite hard to reach, ” Sutherland said.
“So this provider here says: ‘How do we find them, we don’t find them in the streets and all that…we don’t know how to connect with them.’”
However, Sutherland said he would push back slightly on such contentions as there are quite a few transgender focused organisations in the country, despite indications from providers that the transgender community were quite difficult to reach.
Limited Training Opportunities On Transgender Health
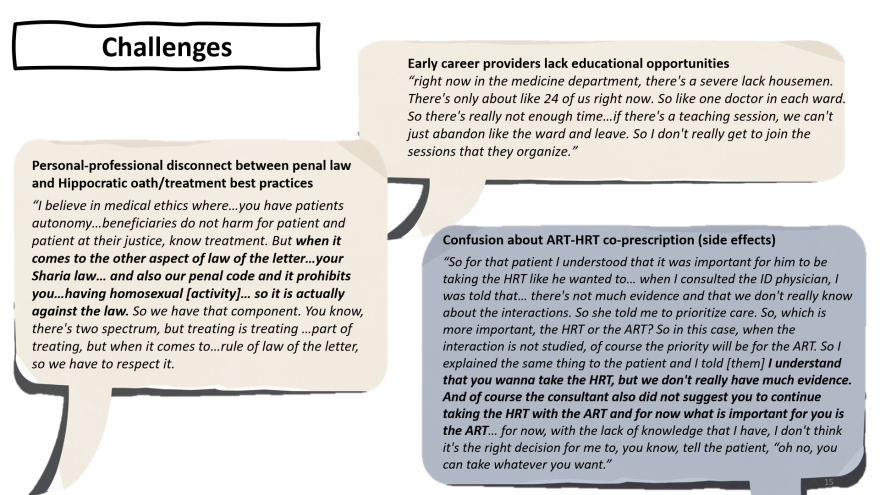
Other challenges mentioned by the providers surveyed were limited training opportunities on transgender health in medical school and beyond.
This can be attributed to the fact that many medical systems have a sort of agreement with specialists, Sutherland said, adding that while specialist care can be beneficial for patients, such systems can lead to some disadvantages for trainee providers.
“The specialists are very good at caring for a specific population if they know what they need and oftentimes transgender patients prefer to go to specialists.
“But this actually left a lot of HOs (house officers) and MOs (medical officers) kind of in the dark about knowing what to do if they met a transgender patient or how to manage their care.
“So, for example, this was one of the representative quotes (from the survey) that we saw: “Transgender care in terms of my undergraduate training, yes, I think I did not receive any training for transgender care.”
In fact, a number of concerns emerged from the study with regards to training on transgender health, which included issues related to content, access, and opportunity, as well as limited target participants.
Sutherland noted that the content presented in some trainings may inadvertently perpetuate discriminatory ideas about transgender and HIV patients.
“Many transgender patients do not have HIV, many HIV patients are not trans, but often within the literature that were shared during these training sessions, they both were conflated and so people might develop some kind of discriminatory thinking when they see those things hand-in-hand all the time during training sessions.”
The shortage of early career providers in Malaysia also impedes the ability of housemen to attend training and other educational opportunities.
A houseman in the study said: “Right now in the medicine department, there’s a severe lack of housemen. There’s only about 24 of us right now.
“So like one doctor in each ward. So, there’s really not enough time…if there’s a teaching session, we can’t just abandon the ward and leave. So, I don’t really get to join the sessions that they organise.”
“So even if there was a session on transgender health or HIV medicine, a lot of these housemen are not able to go and receive the training for continuing medical education,” Sutherland said.
He pointed out that a lot of the training sessions were focused solely on physicians although they are not the only providers in the office.
“There is the phlebotomist, the nursing staff, even the people who are non-providers like the receptionists. And a lot of physicians do not know that these training only target physician providers and miss quite a lot of non-medical staff, which is a missed opportunity.”
ART Or HRT?

The lack of education and knowledge on transgender health care can also create confusion when treating transgender patients, especially when it comes to prescribing ART and hormone replacement therapy (HRT).
Some transgender individuals take hormone therapy as part of their gender transition to help their bodies and appearance align with their gender identity.
A provider in the survey said that while they understood that it was important for a patient they were treating to be taking HRT like he wanted, the infectious disease physician they consulted told the provider: “There’s not much evidence and we don’t really know about the interactions.
“So she told me to prioritise care. So, which is more important, the HRT or the ART?” asked the provider, who concluded that with their lack of knowledge, “I don’t think it’s the right decision for me to tell the patient: ‘oh no, you can take whatever you want.’”
Deficiency in knowledge on prescribing HRTs points to a need for better gender guidelines or clinical practice guidelines (CPGs) in Malaysia, said Sutherland, adding that some of the providers did not know when they were designing the CPGs that the guidelines are discriminatory.
“This comes from the interview data that the providers provide,” said Sutherland, “(There) was very limited conversations with civil organisations, transgender communities as this provider said: ‘To be honest, the consultations only were done through religious organisations with regards to conversion therapy.'”
However, even without adequate local guidelines, there are alternative international guidelines that can help inform trangender treatment and care.
“There are many alternatives from the National Health Service in the UK, US, Australia, but oftentimes there is a general unwillingness to consult international guidelines when it comes to HRT,” he said, adding that this was not the experience with all providers though.
Many Forms Of Stigma

Stigma surrounding the transgender community is another major issue that needs to be addressed based on the research.
“There were several different types of stigma manifesting in provider responses. There was social stigma where doctors didn’t want to be stigmatised to say things or help trans patients because of their sort of professional discomfort,” Sutherland said.
There was also stigma rooted in religion, noted Sutherland providing the following quote by a provider as an example: “I can’t tell them I feel bad because, as a Muslim you’re required to abide by these things that…anything that is LGBT or trans related is against the religion.”
“Quotes like that and it wasn’t just limited to the Muslim experience. It was religion in general,” he maintained, adding though that “there were also people who said that religion was not at all a barrier.
“So I’m just focusing now on several aspects of stigma that did manifest but I’m not singling out any religion or any sort of conviction. In fact, there were multitudes of experiences here.”
Stigma can also be political in nature with some providers saying that the political climate and controversies around the topic has made it very difficult for them to perform their work optimally and treat transgender patients.
“There were also things that happened with them in clinical encounters or behind closed doors that were stigmatising,” Sutherland said.
“Talking behind closed doors among provider communities, there were some conservations about anti-LGBT sentiments and how that might influence prescribing habits.”
He provided the example of a provider who attended a national conference where an endocrinologist stood up and said, “can you promise us that you’re never going to give PrEP to gay people?
“That’s an example of an overt aspect of an anti-LGBT sentiment and how that (stigma) might influence prescribing patterns, not only for PrEP but also for ARTs for this population.”
Counselling For Abstinence, Against Pre-Marital Sex

Stigma also materialised in counselling sessions that were conducted during appointments when treating patients with HIV.
These included counselling against pre-marital sex and risk behaviours, advocating for abstinence — that went beyond a justice and rights based approach.
“Counselling seems to be something that a lot of providers think is appropriate, which it is. Obviously counselling is important, but a lot of the counselling framing was against pre-marital sex, (for) abstinence, it wasn’t rights based. There was some mention of conversion therapy as well.”
Physical Manifestations Of Discrimination

There were also physical manifestations of discrimination, said Sutherland, who also has a Master of Philosophy in Development Studies from the University of Cambridge.
“For example, excessive contact precautions like wearing double gloves when treating or examining a patient.
“I understand that double gloving is something that some medical communities recommend for needlestick injuries but this example here (from the presentation) of wearing double gloves was actually during an exam. It wasn’t during a procedure that required blood to be drawn.”
He added that provider motivated or mediated stigma goes beyond just doctors, and also includes the paramedical staff and people like receptionists, phlebotomists, and community pharmacies, necessitating more comprehensive training about discrimination, and stigma.
“Wording, jargon, things that providers use to describe lifestyles, things like the quote ‘against nature’, providers using trans and homosexual derogatory language around these lifestyles express the fact that acceptance is not just an issue within the community at large, but within the medical community as well.”
On a more positive note however, Sutherland said there were many providers within the sample who were actively fighting to expand the opportunities for more comprehensive rights based transgender and HIV medicine.
“ART Is A Price Killer”

The final section of Sutherland’s presentation focused on providers’ perceptions and opinions of pill training, which is the process of prescribing vitamin pills in lieu of ARTs.
“A vitamin pill is used to build adherence so it is seen by some to improve the habit of taking the medicine, which ART requires you to do.”
His research found that there was a prevailing notion that ARTs are scarce and expensive.
“Obviously pill training originated as a form of ensuring that a costly and scarce medicine was appropriately rationed within society. Now, the medication is quite cheap, but this sort of mentality still remains.
“In fact, a provider said: ‘And obviously, to myself I believe there are also patients who are non-compliant, maybe around 10 to 15 per cent… because the ART is a price killer… I believe if the patients are not willing to take ART, why do we (not) substitute it to other people because it’s taxpayer money, so (it is not good for) our HAART (highly active antiretroviral therapy) to be wasted just like that.’”
Providers who felt positively about pill training believed that it built habits or that it was used to buy time while they were waiting for confirmatory tests.
“Often, confirmatory tests took between two weeks and two months to come back and within that interim period, a lot of providers waited for confirmatory testing and waited by prescribing a vitamin in the interim period,” Sutherland said.
“The two month waiting period happened in places that were not KL, these were places with one IV specialist, a place where they would require sending samples out for analysis — that was obviously not in metropolitan KL.”
While the study found that there was an understanding that longer courses of prescribing vitamin pills may be useful for patients who are unwilling to accept their diagnosis, as a training tool to prompt them and prepare them for taking ART, there were also providers who opined that ART should not be delayed.
As one of them said: “We stopped using vitamin training. I think our main goal is to start ART as soon as possible for these kinds of patients”.
Sutherland said there was also confusion surrounding the way patients were being prescribed pill training, routines, regiments and the way they were being prescribed ART.
“So this provider actually said something very interesting: ‘Part of the pill training which is in the form of vitamins involves patients, from what I’ve been told, taking it twice a day. But we’ve really moved towards a once-a-day pill combination.
“So, you know in that period of two weeks, they’re taking it twice a day, then they move to once a day and then they actually start ART. So, it’s actually kind of confusing to the patient.’”
Sutherland added that local hospital systems may have SOPs that mandate pill training, and physicians may not actually have a role in it.
“It might be led by pharmacists and pharmacies may be the one who are establishing pill duration, and sort of referring back to the physicians once the patient has completed this training programme to then being able to take the ART full time.”
Pill Training Has Both Proponents And Detractors

In summary, Sutherland said based on the study, there were a variety of views on pill training.
“They’re not one simple streamlined viewpoint of pill training. Pill training has both proponents and detractors. Some people really don’t know too much about it, honestly, and that has more to do with when they were trained and that has more to do with the newer trained physicians here.
Sutherland maintained that many physicians also said that vitamin training leads to loss of follow-ups and dropouts.
“They noted that when they prescribed the vitamin to patients, all of those patients did not come back.”
He said there was also a view that vitamin training might foster mistrust between patient and provider.
“Especially with providers engaging in pill counting, which is having the patient after completing their regiment, bring back the bottle of vitamins and checking how many is left, just to see if they’ve been taking them as prescribed.”
Recommendations For Improving Treatment And Care
In conclusion, Sutherland offered some recommendations to improve treatment and care of transgender patients.
He maintained that mental health and counselling services should be expanded to include services that are trauma informed and not affiliated with any conversion therapy.
Additionally, there should be more education on managing side effects for dual prescriptions of ART and HRT.
“Many providers talked about the fact that a lot of patients are going to Thailand or other countries or getting these medications online. Or they went to Thailand for gender affirming surgery.
“And there was very limited understanding of how to manage hormones or surgical complications so I really do feel that there needs to be more education in managing these aspects of care because obviously these patients are going to get these medications anyway so it is a good idea to get educated about these medicines and what their sides effects are.”
He also highlighted the importance of improving training around SOGI (sexual orientation and gender identity).
“There was a large gap in sexual understanding or discomfort in sexual history taking. Malaysian CPGs should be improved and expanded so they include evidence-based sections on transgender health and LGBT health,” Sutherland said, adding that increased training should not be targeted at just physicians but also paramedical staff.
To address the poor attendance at training sessions, Sutherland recommended making them more accessible by offering virtual training sessions.
“A lot of times the training sessions were poorly attended and this was not necessarily because physicians were disinterested in going for them. They often talked about barriers to these sessions.
“If they were in-person, often it would require them to take time off from work, travel, or pay for attendance. Many preferred virtual sessions as it were during the pandemic, as well as opportunities for them to easily access these sessions through guidebooks, resources, things like that.”
He added that training should be non-stigmatising and include opportunities for early learners to practise their skills through the objective structured clinical examination (OSCE).
“That’s a testing style where often medical trainees or students are given a standardised patient. This person is sort of an actor, who is able to talk through different complications and students are able to learn from that through feedback.”
Community involvement of key populations in education and training is also crucial, said Sutherland, adding that credentials for training should also be provided.
“Obviously this is already done but I think post-test training is very important to ensure that knowledge is accurately transmitted and sort of requires multi-agency approaches to training.” He also said opportunities for training that are beyond the medical education world and also involve the community broadly should be expanded.
Finally, Sutherland opined that pill training should probably be phased out.
“I don’t see it as a valuable training opportunity, except for opportunities where patients may have an issue with swallowing — pill training might be useful in those situations.
“Obviously, this is a case-by-case basis, but I think the WHO guidelines are very clear that ART should be started asap for patients who do test positive for HIV.”












